Adhesions prevention
WHAT CAN BE DONE TO PREVENT ADHESIONS?
Although there is no way to eliminate the risk of adhesions completely, there are steps your surgeon can take to reduce the likelihood of adhesion formation.
The most effective methods of adhesion prevention involve meticulous surgical technique and the use of a physical barrier to separate tissue surfaces while they heal.
MICROSURGICAL TECHNIQUES
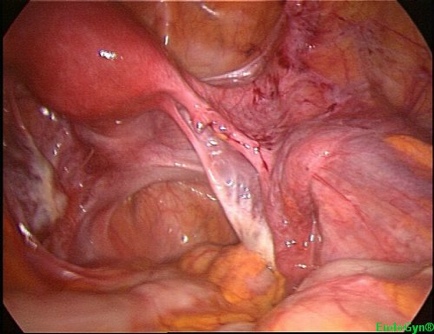
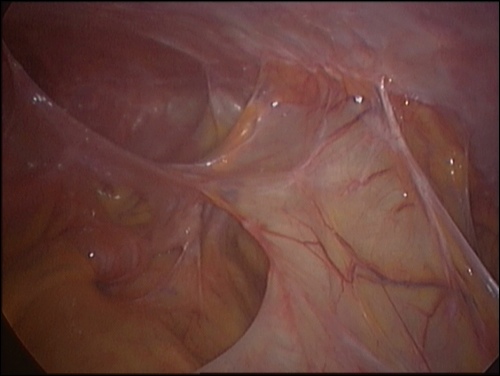
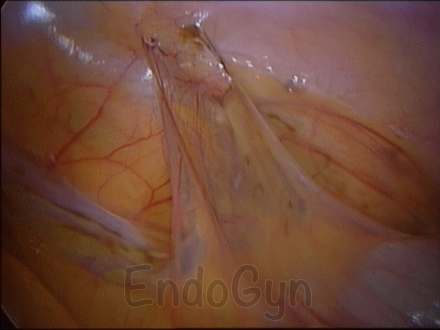
Surgeons have developed microsurgical techniques that minimize trauma, ischemia, foreign bodies, hemorrhage, raw surfaces and infection to reduce adhesion formation.
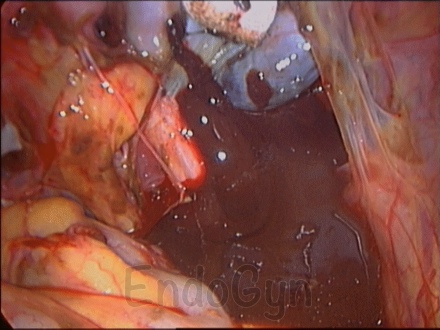
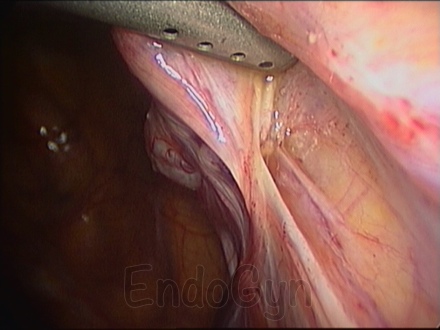
Minimally invasive techniques such as the laparoscopy, that are designed to minimize trauma, blood loss, infection, and the introduction of foreign bodies, all of which can lead to inflammation and adhesion formation.
Good surgical technique involves minimizing tissue handling, using delicate instruments, and keeping the tissues moist when they are exposed to the air.
Surgical techniques that can help decrease adhesion formation
- Achieve meticulous hemostasis
- Maintain vascularity
- Moisten tissues
- Avoid dry sponges
- Minimize tissue handling
- Use fine, non-reactive sutures
- Avoid peritoneal grafts
- Minimize foreign bodies
Not simply the surgical procedure used, but in combination with these techniques and the minimal invasive surgery, i.e. laparoscopy, one has the best chance of adhesion reduction when used in combination.
While good surgical technique is important, but it is often not sufficient to prevent adhesions.
Even though the most meticulous surgical and microsurgical techniques cannot eliminate the formation of adhesions, the other steps can be taken to reduce adhesion formation further are:
- Achieve meticulous hemostasis: Inadequate hemostasis and the resultant fibrin deposition promote adhesion formation.
- Maintain vascularity: Limiting ischemia supports fibrinolysis.
- Moisten tissues:Frequent irrigation and the use of moist sponges prevent desiccation of tissue.
Ringer’s lactate or other irrigating solutions also eliminate any residual talc, lint, or blood clots, which may provide a nidus for a foreign body reaction, inflammation, and adhesion formation. - Avoid dry sponges: Use of gauze and dry sponges should be avoided because they may damage the peritoneal surface and leave a foreign body behind.
- Minimize tissue handling:Manipulating tissue increases the possibility of vascular and tissue damage.When direct manipulation of the peritoneum is necessary, use either atraumatic instruments or fingers.In addition, cutting and coagulating should be kept to a minimum to reduce the possibility of trauma and maintain vascularity.
- Use fine, nonreactive sutures:To minimize foreign body reactions use the smallest size of suture composed of synthetic material.
- Avoid peritoneal grafts:Grafting increases the risk of peritoneal trauma while decreasing vascularity.
- Minimize foreign bodies: Foreign bodies may damage the peritoneal surface, lead to inflammation, and ultimately result in adhesion formation.
Chemical Methods
Various drugs have been evaluated in an effort to reduce the post-operative incidence of adhesions.
To date, no well-controlled study has documented the efficacy of these drugs.
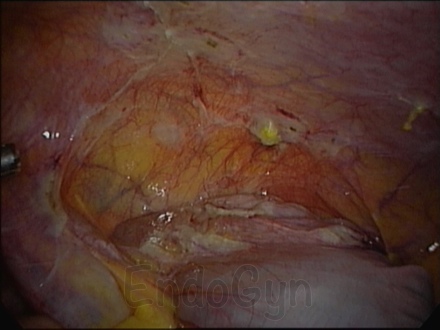
Barrier Methods
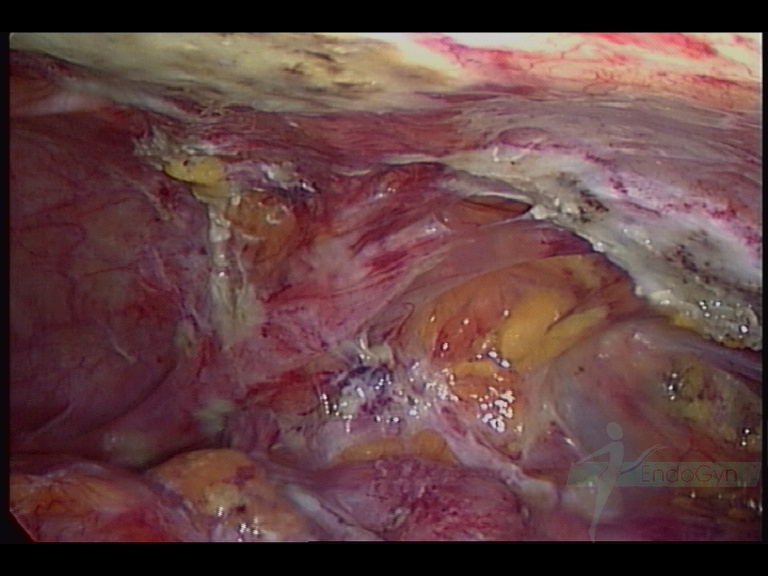
The use of a barrier between raw tissue surfaces appears to be one of the most promising methods of adhesion prevention.
Barriers mechanically separate the surgical surfaces and keep those surfaces apart.
WHAT ARE THE DIFFERENT TYPES OF ADJUVANTS USED TO PREVENT ADHESIONS?
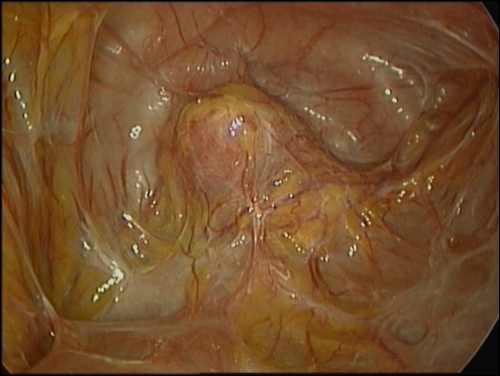
Adhesion formation and reformation are still an unavoidable event in reproductive pelvic surgery in spite of the variable skills in microsurgery and endoscopic surgery.
This fact necessitates the search for barrier that can be used in the perioperative period.
There have various barriers or adjuvants that have been used but none have conclusively proven to be effective in various studies.
CLASSES OF ADHESION-REDUCTION ADJUVANTS AND THEIR PROPOSED MECHANISM OF ACTION
I. Fibrinolytic agents (fibrinolysis, stimulation of plasminogen activators)
Fibrinolysin
Streptokinase
Urokinase
Hyaluronidase
Chymotrypsin
Trypsin
Pepsin
Plasminogen activators
II. Anticoagulants (prevention of clot and fibrin formation)
Heparin
Citrates
Oxalates
III. Anti-inflammatory Agents (reduce vascular permeability, reduce histamine release and, stabilize lysozomes)
Corticosteroids
Nonsteroidal anti-inflammatory agents
Anti-histamines
Progesterone
Calcium channel blockers
Colchicine
VI. Antibiotics (prevent infection)
Tetracyclines
Cephalosporins
V. Mechanical Separation (surface separation, hydroflotation)
A. Intra-abdominal Instillates:
Dextran
Mineral oil
Silicone
Vaseline
Crystalloid solutions
Carboxymethylcellulose
Hyaluronic acid
Chelated hyaluronic acid
Poloxamer
B. Barriers:
Endogenous tissues:
Omental grafts
Peritoneal grafts
Bladder strips
Fetal membranes
Exogenous materials:
Fibrin glue
Polytetrafluoroethylene
Oxidized cellulose
Oxidized regenerated cellulose
Gelatin
Rubber sheets
Metal foils
Plastic hoods
Modified from Diamond MP, DeCherney AH: Pathogenesis of adhesion formation/reformation: Application to reproductive pelvic surgery. Microsurgery 1987: 8: 103 and Diamond MP, Hershlag A: Adhesion formation/reformation: in Treatment of postsurgical Adhesions, Wiley-Liss, Inc. 1990: 23-33.